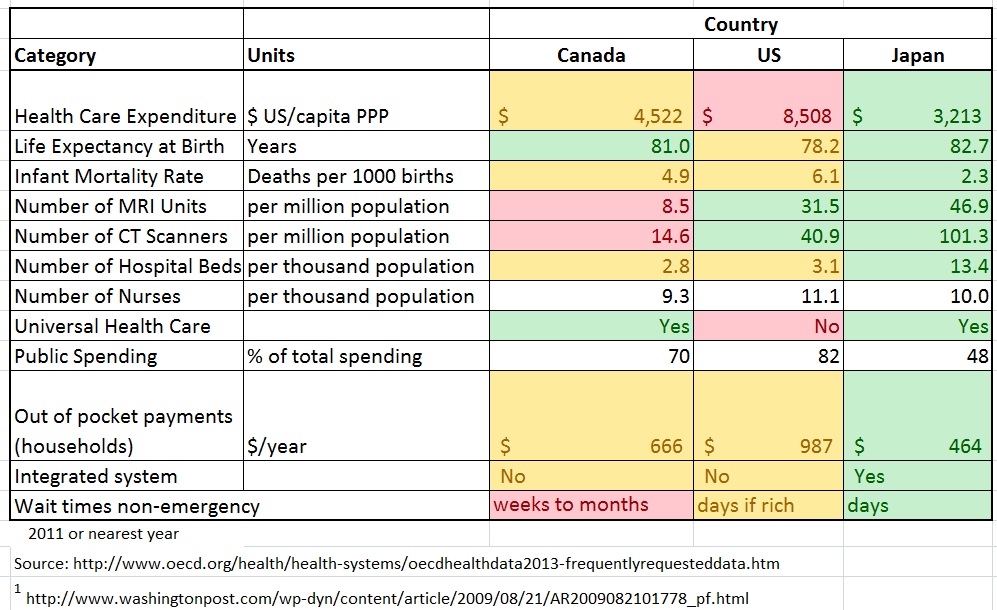
After my recent in-depth experiences with both the Japanese and Canadian Health Care systems, I’ve continued my investigation why the Japanese system has dramatically reduced wait times, better outcomes, and lower costs as compared to the Canadian system. I have included the US system as well. It is clear to me that applying systems engineering to health care will both improve the system and lower its costs. When I experienced the Japanese health care system, I was so shocked at how much better and faster it was than the Canadian system, I wrote a post on it in Sept 2013, and I repeat one of the key tables here:
In Canada, the wait times for critical diagnoses are getting worse (see this recent article in the Globe and Mail). Cancer diagnosis can take 1 to 6 months (!!!) in BC whereas in Japan it can often be done in one day.
The US is getting serious about applying Systems Engineering to their Health Care System. The White House’s President’s Council of Advisors on Science and Technology (PCAST) has published an excellent report in May of 2014 called “Report to the President, Better Health Care and Lower Costs: Accelerating Improvement through Systems Engineering”. The Report is an excellent read and is surprisingly bold in its recommendations. One of the main recommendations is to transition from a fee-for-service model, which is a disincentive to efficient care, to one that pays for value instead of volume.
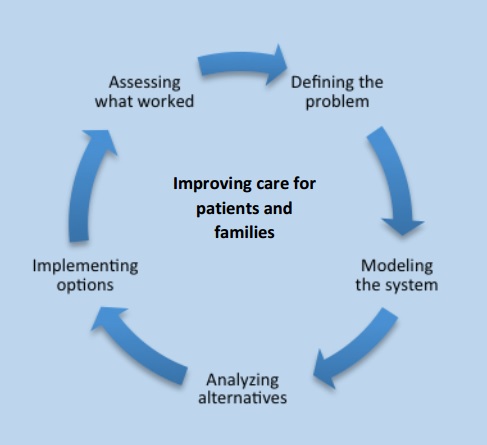
Health Care Systems are very complex, with evolving medical science and technology, multiple stakeholders, increased specialization, and rising expectations of what can be done to treat illnesses, and a lot of realpolitik. Systems engineering has been used successfully and widely in many other complex industries, such as manufacturing or aviation. Systems engineering has also been used to good effect in health care, but too rarely and not widely, and barely at all on the macro scale.
The need to improve health care is required, with increased population, aging, and budgetary pressures. The opportunity for improvement is massive. In the US, approximately 33% of health care costs are wasted, 20-33% of hospitalized patients experience a medical error with about half of them preventable, many quality issues, and caregivers and patients do not have enough necessary information when needed. In Canada, we see many of the same issues as the US, and while we have Universal coverage, wait times for necessary diagnostics or treatment are unnecessarily and often crazily long. Even in Japan, with its worldwide overall best outcomes, low costs, and low wait times, significant improvements are possible in overall efficiency, information flow, costs, and caregiver conditions.
Examples of how systems engineering can improve health care include:
- Denver Health saving $200 million in 2006 by doing a systems redesign of their operations. As an example to reduce waste, one industrial engineer found the trauma surgery resident physicians walk 8.5 miles in a 24 hour shift!
- Kaiser Permanente identified 3x as many sepsis cases and cut mortality from sepsis by 50%
- Virginia Mason has the lowest rate of serious medical infections and falls and reduced medical malpractice liability by 40%
How impactful could systems engineering be if applied at all levels of Health Care? The promise is outcomes as good as Japan or the top tier American care, Universally applied, and lower costs to Government and Patients, with essentially no wait times. It won’t happen overnight, but with the right strategy we could get there in 3-5 years. It is very feasible – if others can do it, we can too. That will then allow us to also be prepared for the greying of our populations. It is good business too, as the improved systems can be exported to other parts of the world. When you have a good system, look how it can dominate the market – like Amazon with its great portal, logistics, and network; or the Internet, with its scalability and extensibility, or air travel with its convenience, low costs, widespread usage, and high safety.
The best studies on how to improve health care by applying systems engineering tools and principles comes from the US. An excellent paper and collection of studies was published in 2005 by the combined efforts of the National Academy of Engineering and the Institute of Medicine called “Building a Better Delivery Systems, a New Engineering/Health Care Partnership”. I highly recommend this paper. Much of this material formed the basis for the 2014 PCAST report to President Obama. Yet one of the last papers in this collection highlights the real difficulties with making improvements in the US Health Care system by analyzing and giving painful examples of the political difficulty, especially with so many interests, organizations and the huge amount of money in the Health Care systems.
Other barriers include:
- Misaligned incentive structure – fee-for-service vs fee-for-outcomes or value
- Availability for data and relevant analytics
- Limited technical capabilities, especially in small practices that make up the bulk of health care
- Workforce competencies – limited knowledge of systems engineering tools and practices
- Leadership / culture / politics
Yet while difficult, governments, organizations, and people around the world understand the need for change, the urgency for change, and that there will be change in Health Care. It is hard work, it will take time, and there are many barriers, especially politically. Slowly and steadily, I expect systems engineering tools, principles, and activities to be applied into the Health Care system. You can help by reading the PCAST and other reports and supporting the application of Systems Engineering to Health Care.
For me, I am approaching Industry, Government and Academic leaders with this message and analysis, participating in consultations, etc.